1. What is Egg Freezing?
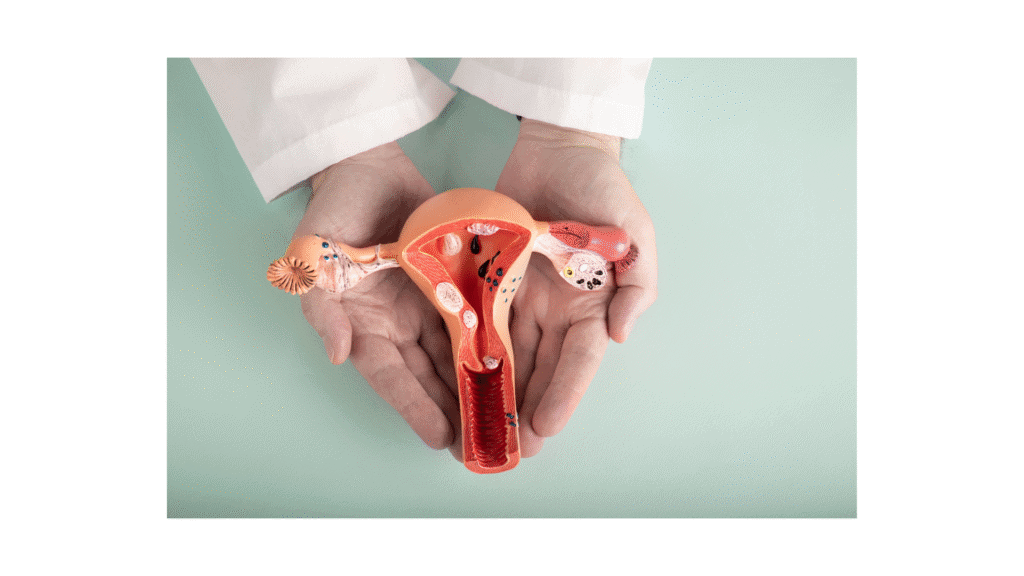
Egg freezing, or oocyte cryopreservation, is a fertility preservation technique that involves:
- Ovarian stimulation to produce multiple eggs.
- Egg retrieval through a minimally invasive procedure.
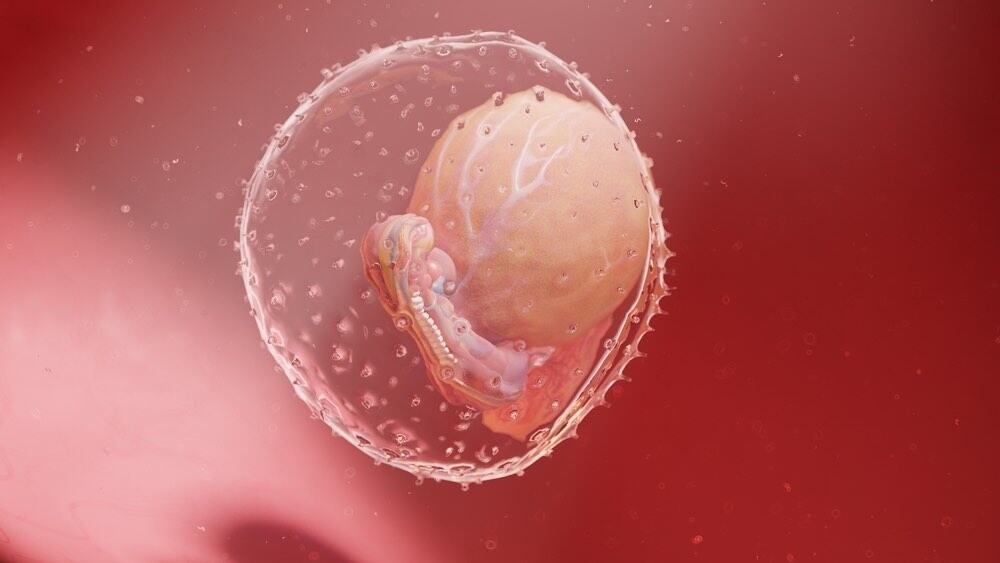
- Cryopreservation (freezing) using vitrification, a fast-freezing method that prevents ice crystal formation, preserving the eggs at extremely low temperatures.
Eggs remain frozen until the individual decides to use them for in vitro fertilization (IVF), at which point they are thawed, fertilized, and implanted into the uterus.
2. Who Should Consider Egg Freezing?
A. Medical Indications
Egg freezing is recommended for individuals who may face fertility loss due to medical conditions or treatments, including:
- Cancer patients undergoing chemotherapy or radiation therapy, which can damage ovarian function.
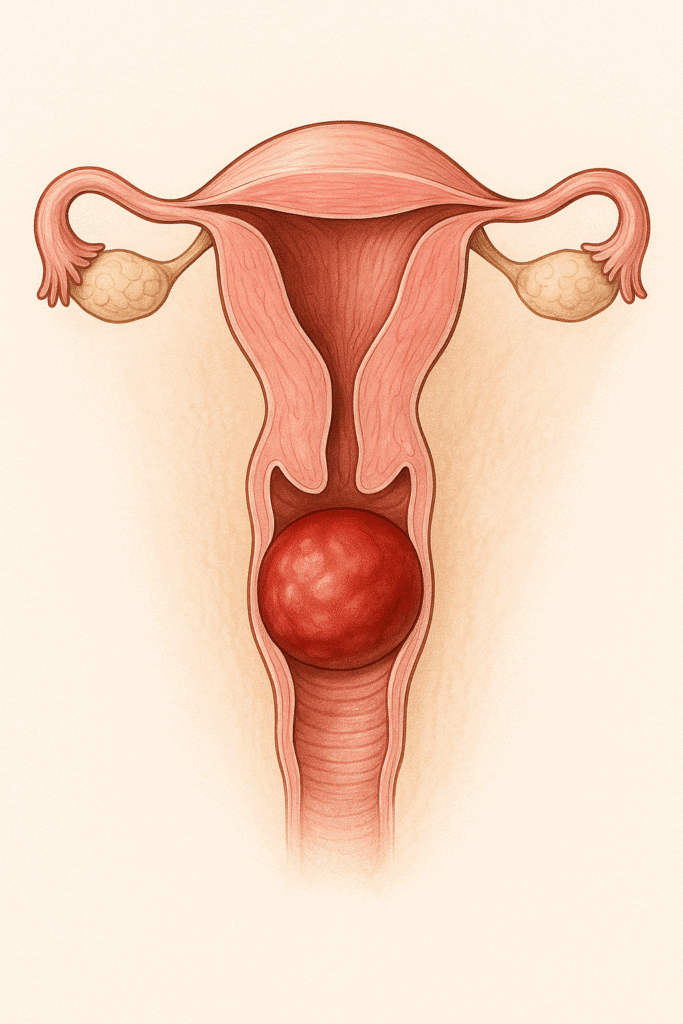
- Endometriosis, a condition that may cause scarring and reduced ovarian reserve.
- Autoimmune diseases (e.g., lupus, rheumatoid arthritis) requiring treatments that affect fertility.
- Genetic disorders, such as BRCA mutations, which may necessitate ovary removal.
B. Social or Elective Freezing
Some women choose to freeze their eggs for personal, career, or relationship reasons to extend their reproductive timeline. Studies show that women under 35 have higher success rates when using frozen eggs later.
Ideal candidates for elective freezing:
- Women in their late 20s to early 30s who want to delay childbearing.
- Those not ready to start a family but concerned about age-related fertility decline.
- Individuals with low ovarian reserve (diagnosed through AMH and antral follicle count testing).
3. Step-by-Step Process of Egg Freezing
Step 1: Fertility Assessment & Hormonal Testing
Before egg freezing, women undergo a comprehensive fertility evaluation, including:
- Anti-Müllerian Hormone (AMH) test – Measures ovarian reserve.
- Antral Follicle Count (AFC) – Assesses the number of follicles available for stimulation.
- Follicle-Stimulating Hormone (FSH) & Estradiol levels – Help determine ovarian function.
Step 2: Ovarian Stimulation (10–14 Days)
- The patient self-administers hormone injections (FSH, LH) to stimulate multiple eggs.
- Regular ultrasound monitoring and blood tests track follicle growth.
- A trigger shot (hCG or GnRH agonist) is given 36 hours before retrieval to mature eggs.
Step 3: Egg Retrieval (Oocyte Aspiration)
- A doctor retrieves eggs using a minor surgical procedure called transvaginal ultrasound-guided aspiration.
- The patient is under mild sedation, and a needle is inserted into the ovaries to extract mature eggs.
- The procedure takes about 15–30 minutes.
Step 4: Vitrification (Fast Freezing of Eggs)
- The retrieved eggs undergo vitrification, an ultra-rapid freezing method that prevents ice crystal formation.
- Eggs are stored in liquid nitrogen at -196°C, maintaining their quality for years.
4. Success Rates of Egg Freezing
The success of egg freezing depends on age, number of frozen eggs, and the clinic’s laboratory techniques.
| Age at Freezing | Chance of Live Birth per Thawed Egg |
| < 35 years | 7–15% per egg |
| 35–38 years | 5–10% per egg |
| > 38 years | 3–5% per egg |
Key Findings:
- Freezing 15–20 eggs before age 35 offers a 70% chance of at least one live birth.
- Younger eggs have higher survival rates and better embryo development after thawing.
- Success rates decline significantly after age 38 due to lower egg quality.
5. How Long Can Eggs Stay Frozen?
- There is no known limit to how long eggs can remain frozen while maintaining viability.
- The longest-reported case of a successful birth from a 14-year-old frozen egg demonstrates long-term storage safety.
6. Risks and Considerations
Medical Risks
- Ovarian hyperstimulation syndrome (OHSS) – A rare reaction to fertility medications that causes bloating and discomfort.
- Egg retrieval procedure risks – Infection or bleeding (rare).
Ethical and Emotional Considerations
- Egg survival is not guaranteed – Not all eggs survive the freezing, thawing, and fertilization process.
- Emotional impact – Some women feel pressure about using or discarding frozen eggs later in life.
7. Cost of Egg Freezing
Egg freezing costs vary by country and clinic, but the average price per cycle is:
| Country | Cost per Cycle (USD) |
| USA | $6,000 – $15,000 |
| UK | £3,500 – £5,000 |
| Europe | €3,000 – €6,000 |
| Australia | $5,000 – $8,000 |
Additional Costs:
- Medications: $3,000–$5,000 per cycle.
- Annual storage fees: $500–$1,000 per year.
- IVF treatment later: $10,000–$15,000.
Some insurance providers and employers now cover egg freezing for medical reasons, and companies like Facebook and Apple offer it as an employee benefit.
8. Conclusion: Is Egg Freezing Right for You?
Egg freezing offers a valuable option for fertility preservation, but it is not a guarantee of future pregnancy. Women should carefully evaluate their age, ovarian reserve, and future reproductive goals before deciding. Consulting a fertility specialist is crucial to understand individual success probabilities.
Key Takeaways
✔ Best done before age 35 for higher success rates.
✔ 15–20 frozen eggs = ~70% chance of live birth.
✔ Costs range from $6,000–$15,000 per cycle, plus storage fees.
✔ New advances continue to improve egg freezing success.
Would you like a personalized fertility consultation? Talk to a fertility expert today!
References:
- Han E, Seifer DB. Oocyte Cryopreservation for Medical and Planned Indications. J Clin Med. 2023;12(3542).
- Varlas VN, Bors RG, Albu D, et al. Social Freezing: Pressing Pause on Fertility. Int J Environ Res Public Health. 2021;18(8088).
- Cascante SD, et al. Planned Oocyte Cryopreservation: The State of the ART. RBMO. 2023;47(6):103367.