At just fifteen, Emily believed her world had collapsed.
Misdiagnosed PCOS:
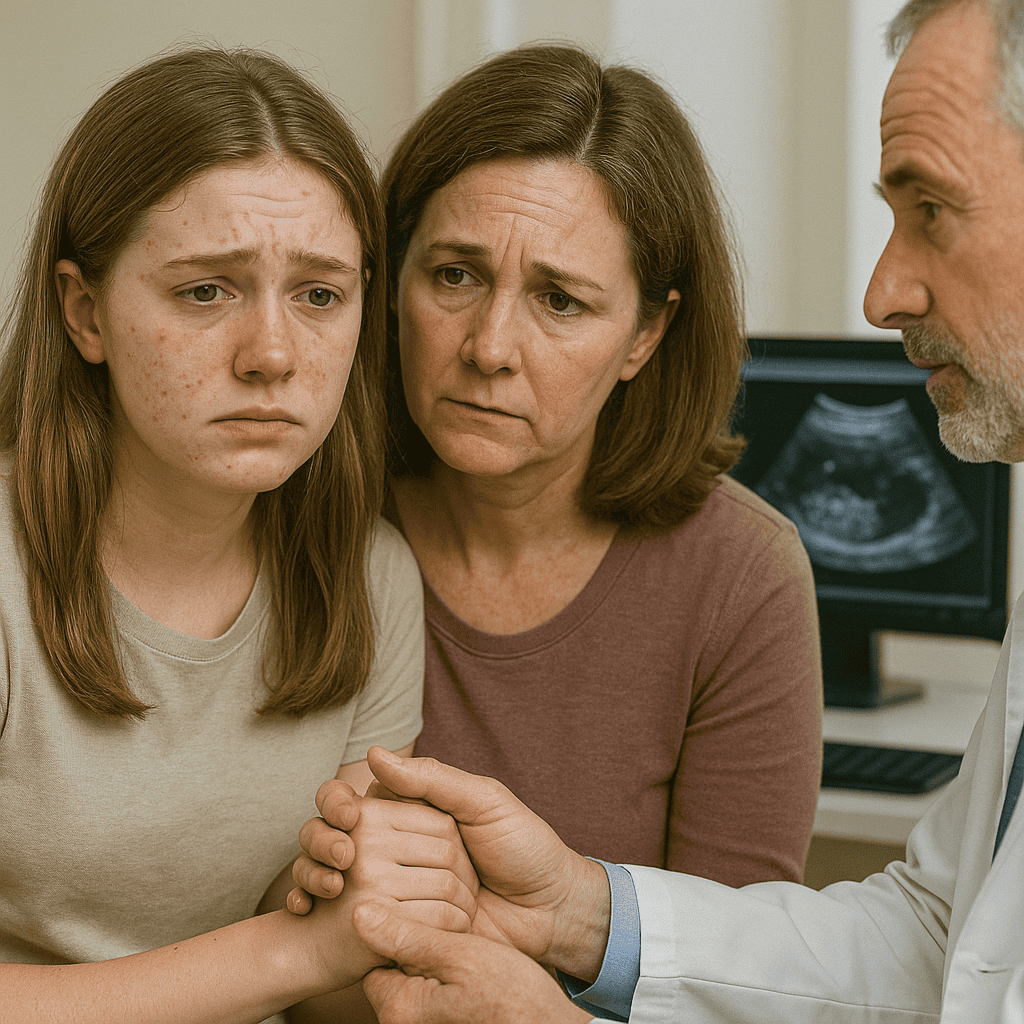
What started as a simple trip to the doctor to investigate irregular periods and persistent acne ended in devastating words: “You have PCOS. You will probably never have children.”
No explanation. No hope. Just a diagnosis delivered with cold finality, leaving a young girl and her mother in silent despair.
Misdiagnosed PCOS: The Power of a Single Sentence
Emily sat in the car after the appointment, staring out the window, numb. Her mother tried to stay strong, but tears slipped down her cheeks. Neither knew much about PCOS — only that it sounded like a life sentence, a closed door at the start of Emily’s adulthood.
Fear took over their home in the days that followed. Emily started Googling late at night, her heart sinking with each new page. Infertility. Weight struggles. Chronic pain. Hormonal chaos. It felt like her future was stolen before it had even begun.
Misdiagnosed PCOS:The Search for Hope
It was Emily’s aunt who, days later, intervened with gentle urgency. “Get a second opinion,” she said. “Not every doctor’s words are final. Especially when they crush hope instead of offering help.”
Reluctantly, Emily and her mother booked an appointment with a reproductive endocrinologist — a specialist who treated adolescent PCOS with a different perspective: one grounded in science, but also compassion.
Misdiagnosed PCOS: Listening, Not Labeling
From the first moment, the second doctor made a difference.
She didn’t rush through Emily’s history. She asked about her first period, her cycle patterns, her skin, her family history, her feelings. She listened — truly listened — not just to symptoms but to fears.
She gently explained that diagnosing PCOS in teenagers was complicated. Irregular periods are normal for a few years after menarche. Hormonal fluctuations are part of growing up. A diagnosis of PCOS could only be made carefully, considering clinical signs, biochemical markers, and persistence of symptoms over time.
And even when PCOS is confirmed, it is not a guarantee of infertility. With proper management, most women with PCOS can conceive — and live full, vibrant lives.
Misdiagnosed PCOS: Understanding Real PCOS
What is PCOS?
Polycystic Ovary Syndrome, or PCOS, is one of the most common hormonal conditions affecting women of reproductive age. If you’ve been told you have PCOS, please know that you’re not alone — it affects an estimated 8 to 13% of women worldwide, and many go undiagnosed for years.
In simple terms, PCOS is a hormonal imbalance that interferes with how your ovaries work. “Polycystic” doesn’t necessarily mean you have cysts — it’s a bit misleading. Instead, the condition is characterized by three main features:
- Irregular or infrequent periods
- Excess male hormones (androgens) in your system
- Enlarged ovaries with many small follicles (immature eggs) seen on ultrasound
You only need two out of these three to be diagnosed.
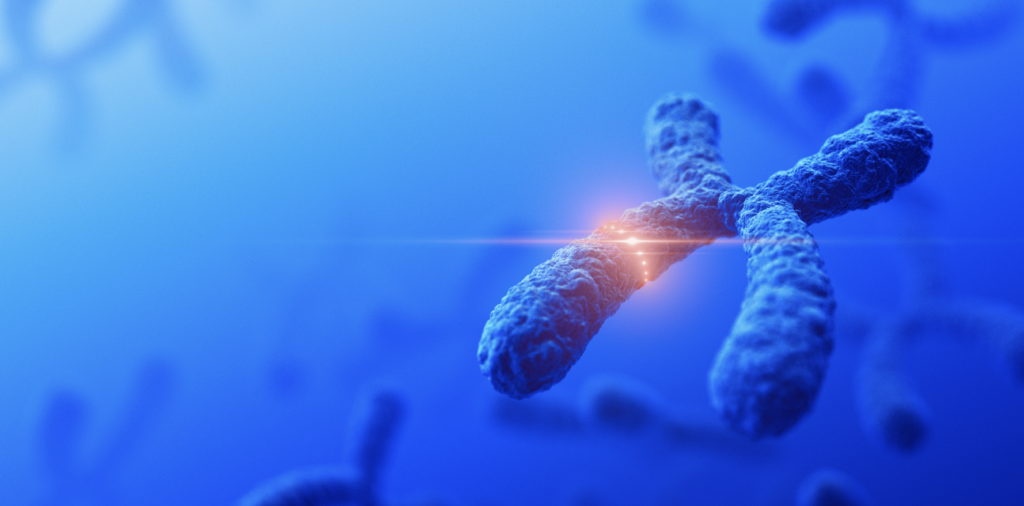
What Causes PCOS?
The exact cause of PCOS isn’t fully understood, but we believe it’s a combination of genetics and environmental factors. If your mother or sister has it, your chances may be higher too. And while it’s not caused by lifestyle, things like weight gain or high blood sugar can worsen the symptoms.
The core issue in PCOS seems to be insulin resistance. This means your body doesn’t use insulin efficiently, leading to higher insulin levels. In response, your ovaries may produce more androgens (male hormones like testosterone), which interfere with ovulation.
That’s why PCOS is often associated with:
- Irregular ovulation
- Fertility challenges
- Acne, hair growth (hirsutism), or hair thinning
- Weight gain or difficulty losing weight
What Are the Symptoms of PCOS?
The symptoms of PCOS vary from person to person. Some women have very mild signs, while others struggle with multiple aspects of the condition. Here are the most common:
1.Irregular Periods
This is often the first sign. You may have fewer than nine periods a year, or cycles that are unpredictable and long (more than 35 days apart). Some women go months without menstruating, while others experience very heavy bleeding when their period does come.
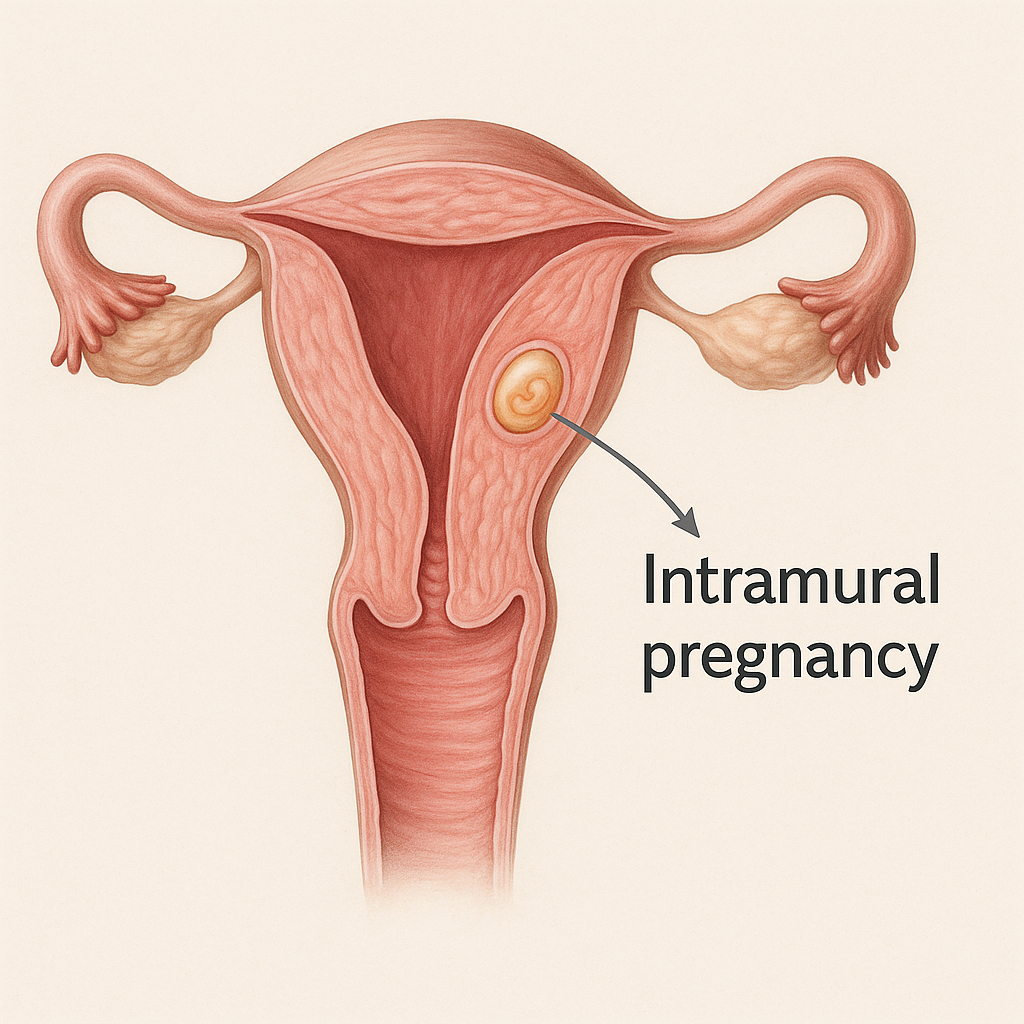
2. Ovulation Problems and Infertility
PCOS is one of the most common causes of ovulatory infertility. If you don’t ovulate regularly, it becomes harder to conceive. But please know that having PCOS doesn’t mean you can’t get pregnant. Many women with PCOS go on to have healthy pregnancies with the right treatment and support.
3. Excess Androgens (Male Hormones)
These can lead to:
- Acne, especially around the jawline
- Excess facial or body hair (on the chin, chest, back, abdomen)
- Hair thinning or male-pattern hair loss
4. Weight Gain or Difficulty Losing Weight
Due to insulin resistance, your body tends to store fat more easily, especially around the abdomen. But not all women with PCOS are overweight — there’s a subtype called “lean PCOS” as well.
5. Darkening of the Skin
Some women notice patches of darker, thicker skin in areas like the neck, underarms, or groin. This is called acanthosis nigricans and is often linked to insulin resistance.
6. Mood Changes
PCOS is not just physical. Many women experience anxiety, depression, or low self-esteem — especially when dealing with body image issues or fertility struggles.
How is PCOS Diagnosed?
PCOS is a clinical diagnosis, meaning we don’t rely on a single test. Instead, we look at your symptoms, your medical history, physical examination, blood tests, and ultrasound findings. We typically use what’s called the Rotterdam Criteria for diagnosis. According to this, you need at least two of the following three:
- Irregular or absent ovulation (e.g., missed or infrequent periods)
- High androgen levels (either measured in blood or evident through acne, hirsutism, etc.)
- Polycystic ovaries on ultrasound (having 20 or more small follicles in one or both ovaries)
We’ll also run blood tests to:
- Check androgen levels (testosterone, DHEA-S)
- Measure hormones like LH, FSH, prolactin, and TSH
- Screen for insulin resistance or prediabetes
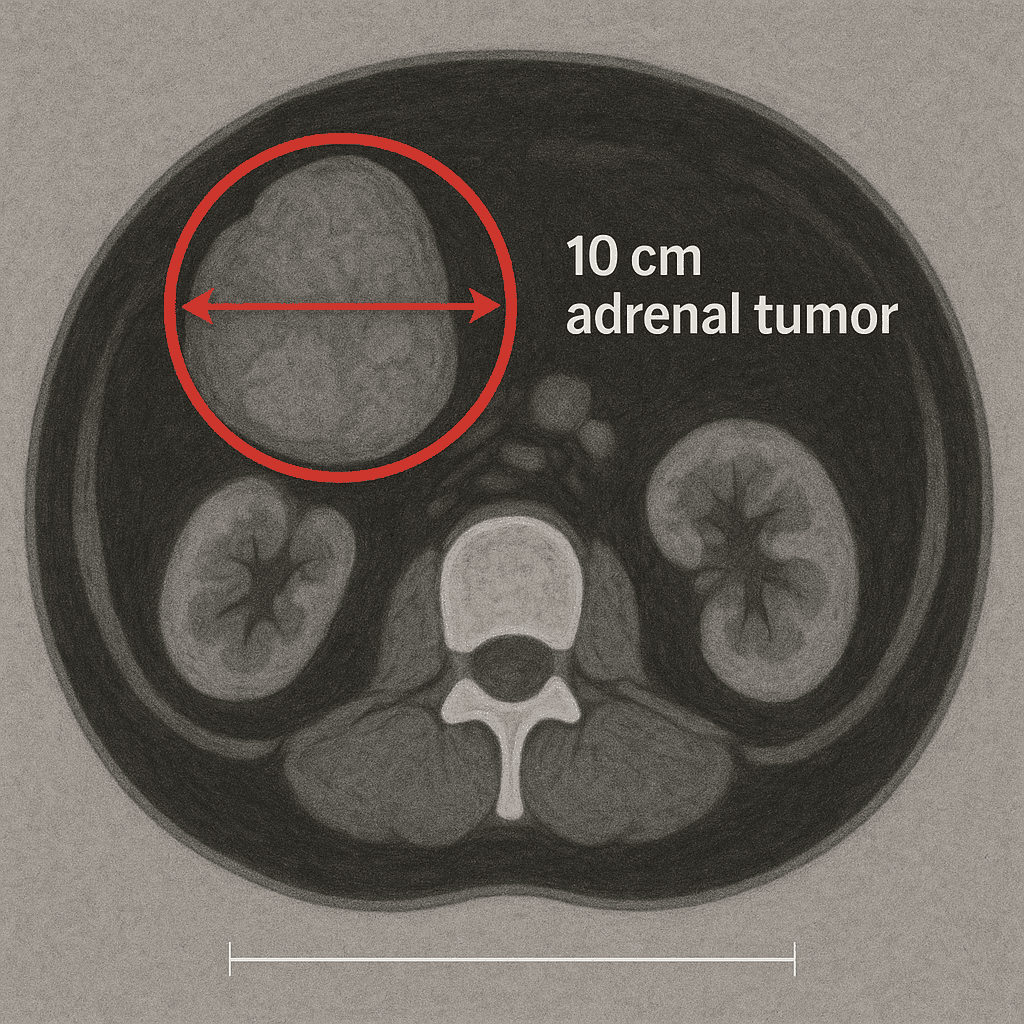
- Rule out other conditions that mimic PCOS, like thyroid disease or adrenal disorders
Is PCOS a Lifelong Condition?
Yes — PCOS is a chronic condition, but it’s manageable. The symptoms can improve with the right lifestyle, medications, and medical guidance. And your needs may change over time — for example, if you’re trying to conceive vs. managing metabolic health later in life.
While PCOS doesn’t go away, it doesn’t mean you’re powerless. Many women find that once they understand the condition and start making changes, their symptoms improve dramatically.
How is PCOS Treated?
There’s no “one-size-fits-all” treatment for PCOS. The best approach depends on your main concern — whether it’s irregular periods, unwanted hair growth, acne, weight, or fertility. Let’s go over the common strategies.
1. Lifestyle Changes (First-line for All Women with PCOS)
Even modest weight loss (5-10%) can restore ovulation, regulate periods, and improve insulin sensitivity. But the goal isn’t just weight — it’s metabolic health.
- Nutrition: Choose whole foods, reduce refined carbs, and eat plenty of fiber, protein, and healthy fats. Some women do well with low-GI or Mediterranean-style diets.
- Exercise: Aim for at least 150 minutes of moderate exercise per week. Resistance training helps with insulin sensitivity.
- Sleep & Stress: Poor sleep and high cortisol levels can worsen PCOS. Try to prioritize rest and manage stress with mindfulness or therapy.
2. Medications (Tailored to Your Goals)
A.
Hormonal Birth Control Pills
These are commonly used if you’re not trying to get pregnant. They:
- Regulate menstrual cycles
- Reduce androgen levels (helping with acne and hair growth)
- Lower the risk of endometrial cancer caused by irregular bleeding
B. Metformin
Originally used for diabetes, Metformin helps with insulin resistance and may:
- Restore regular periods
- Improve fertility
- Support weight loss It’s especially helpful for women with signs of prediabetes.
C. Spironolactone
This anti-androgen blocks the effects of testosterone. It’s used to treat hirsutism and acne, but can’t be used during pregnancy, so effective contraception is required.
D. Letrozole or Clomiphene
These are ovulation induction medications used if you’re trying to conceive. Letrozole is now considered more effective than Clomid for many women with PCOS.
E. Other Options
- Inositol (Myo- & D-Chiro Inositol): Natural supplements that improve insulin sensitivity and ovulation.
- GLP-1 receptor agonists: Newer medications for weight loss and insulin control (e.g., semaglutide).
3. Hair and Skin Management
For excess hair, acne, or hair thinning, we may recommend:
- Topical creams (like eflornithine)
- Laser hair removal
- Prescription acne medications
- Nutritional support like zinc or omega-3
This area of treatment often combines dermatology and endocrinology.
What About Fertility?
Having PCOS does not mean you’re infertile — but it can make it harder to conceive without support. Since ovulation is irregular or absent, you may need help getting your cycles back on track.
Steps might include:
- Lifestyle changes
- Tracking ovulation (apps, OPKs, or ultrasounds)
- Ovulation medications (like Letrozole)
- In some cases, IVF is used — but usually not as a first option
Many women with PCOS conceive naturally once their cycles are regulated, and many others get pregnant with mild assistance.
Long-Term Health and PCOS
PCOS is not just about periods or acne. It can affect your long-term health. That’s why ongoing care is so important.
Women with PCOS are at increased risk for:
- Type 2 diabetes and prediabetes
- High blood pressure
- High cholesterol
- Endometrial (uterine) cancer
- Sleep apnea
- Depression and anxiety
The good news? All of these risks can be managed — especially with early action.
Your healthcare provider should monitor:
- Your weight and waist circumference
- Blood pressure
- Blood sugar (A1C or fasting glucose)
- Cholesterol
- Mental health and mood
Misdiagnosed PCOS:
The second doctor ordered blood tests — testosterone, DHEA-S, fasting insulin — and reassured Emily that the results would guide decisions, not guesses.
Misdiagnosed PCOS: The Truth Behind the Symptoms
When Emily’s results came back, they showed mildly elevated androgens — not unusual for a teenager. Her insulin was normal. Her ovaries, seen by ultrasound, showed no signs of enlarged volume or cystic appearance.
It was clear: Emily didn’t have PCOS at all. She had normal pubertal changes, slightly delayed, that would likely resolve on their own or with minimal hormonal support if needed.
The “infertility” label had been wrongly placed on a growing, healthy teenager who needed patience, not panic.
Misdiagnosed PCOS: The Emotional Healing Begins
Hearing the second doctor’s calm explanation was like breathing again after weeks underwater. Emily cried, but this time with relief. She wasn’t broken. Her body wasn’t doomed. She wasn’t destined for loss before she had even lived.
The trauma of the first misdiagnosis didn’t vanish overnight. Trust takes time to rebuild. But with education, support, and kindness, Emily began to heal — inside and out.
Misdiagnosed PCOS: What Happens When We Label Too Fast
Emily’s story is far from unique. Around the world, young girls are often mislabeled with serious diagnoses without proper evaluation. The impact is not just medical — it’s deeply emotional:
- Fear of the future
- Shame about their bodies
- Anxiety and depression
- Distrust in healthcare
Words matter. How doctors communicate, especially with young patients, can either empower them or devastate them.
Misdiagnosed PCOS: The Power of Second Opinions
Second opinions are not about mistrusting doctors — they are about protecting hope and ensuring thoroughness. In conditions like PCOS, where diagnosis is complex and management affects a woman’s entire future, confirming findings is not just reasonable — it’s responsible.
Misdiagnosed PCOS: Education Is the Antidote
Emily now speaks openly to friends facing hormonal struggles: “Ask questions. Find doctors who explain, not just prescribe. You deserve answers you can understand — and options that give you strength.”
At VitaFemme, we believe that every woman, at every age, deserves that same respect.
Misdiagnosed PCOS: Takeaways for Young Women and Families
- Don’t panic after a single diagnosis, especially in adolescence.
- PCOS is common, but so are normal pubertal variations.
- Management is possible. Hope is real. Fertility is often preserved.
- Empower yourself with information and compassionate care.
Misdiagnosed PCOS: Emily’s Message to Every Girl Facing Fear
You are not your diagnosis. You are not broken. Your future is bigger than one consultation, one misjudgment. Trust your body. Trust your journey. And never be afraid to seek a second voice.
Living with PCOS can be overwhelming. The symptoms are visible and invisible — affecting your body, your self-esteem, your future. But I want you to hear this clearly:
There is support. There is treatment. And there are many paths forward — whether your goal is to have a baby, improve your skin, or simply feel better in your body.
Talk to your doctor, ask questions, and don’t settle for being dismissed. You deserve answers and a care plan that makes sense for your life.
Together, we can manage PCOS — not just with medicine, but with compassion, knowledge, and empowerment.
▶️ Listen to Emily’s Full Story on VitaFemme Podcast
Misdiagnosed PCOS: References
- GOODMAN, N.F. et al. Diagnosis and management of polycystic ovary syndrome: An Endocrine Society clinical practice guideline. The Journal of Clinical Endocrinology & Metabolism, 2015.
https://doi.org/10.1210/jc.2015-2465
- WITCHEL, S.F. Polycystic Ovary Syndrome in Adolescents. Frontiers in Hormone Research, 2018.
https://doi.org/10.1159/000491504
- TEDELA, S., et al. Diagnostic challenges of polycystic ovary syndrome among adolescents. Journal of Pediatric and Adolescent Gynecology, 2020.
https://doi.org/10.1016/j.jpag.2020.07.009
- HART, R. & HICKEY, M. Long-term health risks in women with PCOS. The Lancet Diabetes & Endocrinology, 2014.
https://doi.org/10.1016/S2213-8587(14)70071-6
- DEWAILLY, D., et al. The spectrum of PCOS in adolescents. Best Practice & Research Clinical Obstetrics & Gynaecology, 2010.
https://doi.org/10.1016/j.bpobgyn.2009.08.002
- VITA, N. A Misdiagnosis of Despair: The Journey of a Young Girl Confronting PCOS. VitaFemme Podcasts, 2025.
https://vittafemme.com/podcast/misdiagnosed-pcos-teen-journey