1. Understanding IVF: Who Can Benefit from IVF?
· IVF is recommended for:
· Women with blocked or damaged fallopian tubes.
· Women with low ovarian reserve or poor egg quality.
· Couples experiencing unexplained infertility.
· Men with low sperm count or poor sperm motility.
· Individuals with genetic conditions requiring embryo screening.
· LGBTQ+ couples and single parents using donor eggs, sperm, or surrogacy.
2.Understanding IVF: How the Process Works
Step1: Ovarian Stimulation
- The woman takes hormonal injections for 10–14 days to stimulate multiple eggs to develop.
- Follicle growth is monitored via ultrasound and blood tests.
- When the follicles reach maturity (17–20mm in size), an hCG trigger shot is administered.
Step 2: Egg Retrieval (Oocyte Aspiration)
- 36 hours after the trigger shot, eggs are retrieved using a thin needle inserted through the vagina, guided by ultrasound.
- The procedure takes 15–20 minutes and is performed under sedation or anesthesia.
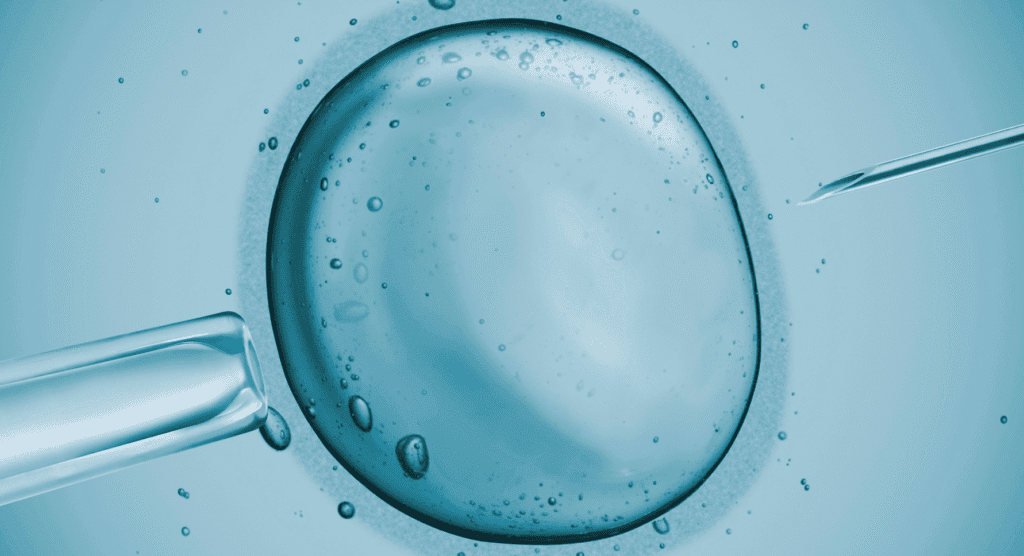
Step 3: Sperm Collection and Fertilization
- A sperm sample is collected from the partner or donor.
- Fertilization is done using one of two methods:
- Conventional IVF – Sperm and eggs are placed together in a petri dish.
- ICSI (Intracytoplasmic Sperm Injection) – A single sperm is injected directly into each egg, often used for male infertility.
Step 4: Embryo Development
- Fertilized eggs develop into embryos over 5–6 days.
- Embryologists monitor cell division and quality.
- On Day 5 or 6, the best embryos (blastocysts) are selected for transfer.
Step 5: Embryo Transfer
- The healthiest embryo(s) are transferred into the uterus using a thin catheter.
- The procedure is quick and painless, similar to a Pap smear.
- Any extra embryos can be frozen for future use.
Step 6: The Two-Week Wait and Pregnancy Test
- 12–14 days after embryo transfer, a blood test checks for pregnancy.
- If positive, pregnancy is monitored via ultrasound at 6–7 weeks to confirm fetal heartbeat.
3.Understanding IVF/IVF Success Rates: What to Expect?
Success Rates by Age
Age Group IVF Success Rate (Live Births per Cycle)
Under 35 45–70%
35–37 40%
38–39 30–35%
40–42 8–25%
Over 42 <10%
IVF is most successful in younger women because egg quality declines with age.
Factors That Affect IVF Success
· Age and ovarian reserve – AMH and follicle count play a key role.
· Sperm quality – Poor sperm motility may require ICSI.
· Uterine health – Fibroids, polyps, or thin endometrial lining can impact implantation.
· Embryo quality – Chromosomal abnormalities lower success rates.
· Lifestyle factors – Smoking, obesity, and stress negatively affect outcomes.
4.Understanding IVF/ Risks and Side Effects of IVF
While IVF is safe, potential risks include:
A. Ovarian Hyperstimulation Syndrome (OHSS)
- Caused by excessive hormone stimulation.
- Symptoms: bloating, nausea, rapid weight gain, fluid retention.
- Severe cases require hospitalization.
B. Multiple Pregnancies
- Transferring multiple embryos increases the risk of twins or triplets.
- Multiple pregnancies lead to higher risks of preterm birth and complications.
C. Emotional and Financial Stress
- The emotional toll of failed cycles can be significant.
- IVF costs range from $10,000 to $20,000 per cycle, depending on location.
5.Understanding IVF/ Cost and Accessibility of IVF
Country. Average Cost per Cycle (USD)
United States. $12,000 – $25,000
UK $7,000 – $10,000
Canada $10,000 – $15,000
Brazil $4,000 – $6,000
India $2,000 – $4,000
· Some insurance plans cover IVF, but coverage varies by country and provider.
6. Conclusion: Is IVF Right for You?
IVF offers hope to many couples facing infertility, but it is not a guaranteed solution.
· Younger patients have higher success rates.
· Embryo freezing allows for multiple attempts.
· Genetic testing (PGT-A) can help identify healthy embryos.
· Emotional support is crucial – consider counseling during treatment.
If you are considering IVF, consult a fertility specialist to discuss your options and personalize your treatment plan.
Would you like to explore the next topic: “Egg Freezing: Who Should Consider It and How It Works”?
References
- Practice Committee of the American Society for Reproductive Medicine (ASRM). "Assisted Reproductive Technology Success Rates." Fertility and Sterility, 2023.“>Practice Committee of the ASRM. “Assisted Reproductive Technology Success Rates.” Fertility and Sterility, 2023.