Best Contraceptive Method
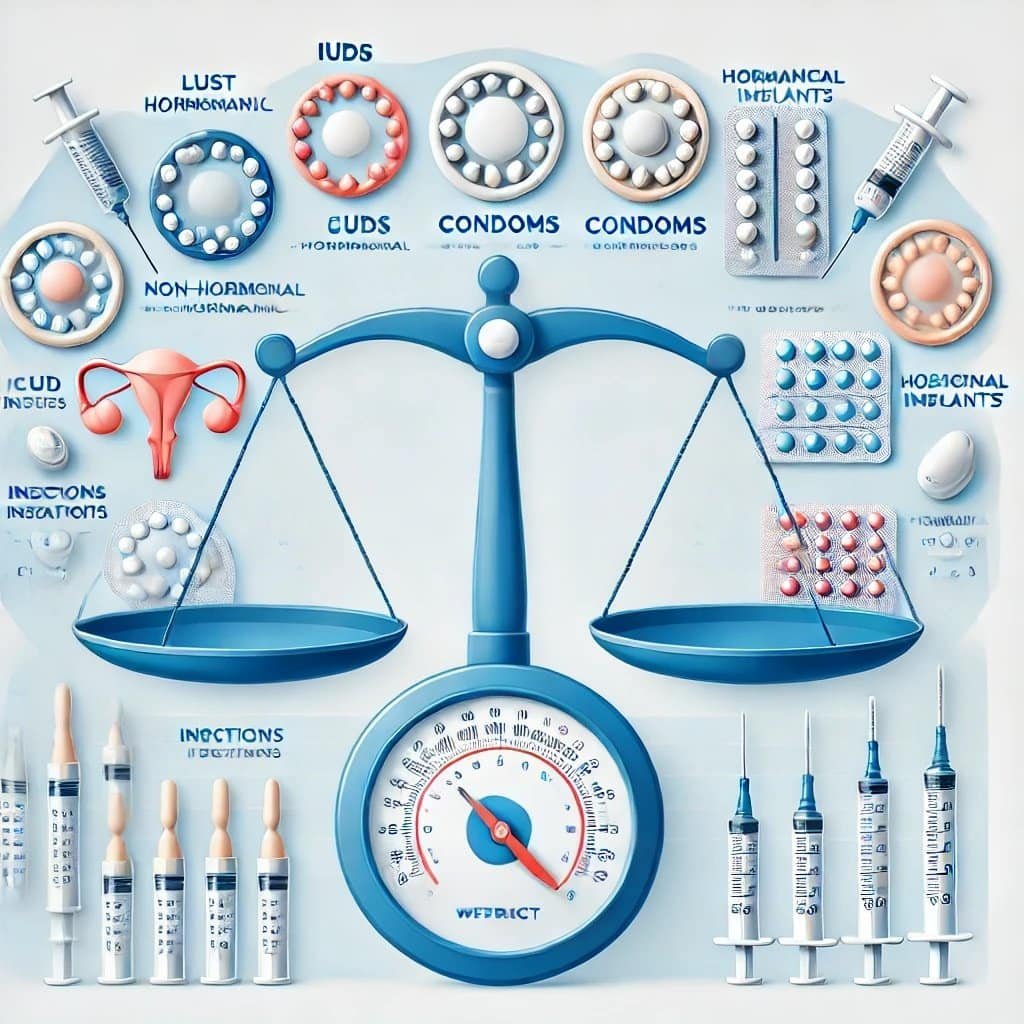
Choosing the best contraceptive method depends on individual needs, health conditions, and lifestyle. While all birth control methods aim to prevent pregnancy, some are more effective, more convenient, or have additional benefits like regulating periods or reducing acne. This article explores different birth control options, their effectiveness, side effects, and factors to consider when choosing the best method for you.
1. What Defines a Best Contraceptive Method?
The best contraceptive method varies from person to person. To determine which is right for you, consider:
Effectiveness: How well does it prevent pregnancy?
Convenience: Do you prefer a daily pill, a long-term solution, or something you don’t have to think about often?
Side Effects: Do you want to avoid hormones?
Health Considerations: Do you have any medical conditions that limit your options?
Future Pregnancy Plans: Do you want a reversible method or permanent birth control?
STI Protection: Do you need a method that also prevents sexually transmitted infections (STIs)?
With these factors in mind, let’s explore the different types of birth control.
2. The Best Contraceptive Methods
If effectiveness is your top priority, these methods provide the best protection against pregnancy:
IUDs (Intrauterine Devices) – Over 99% Effective
IUDs are small, T-shaped devices inserted into the uterus. They are one of the most effective and long-lasting forms of birth control.
- Hormonal IUDs
- Lasts 3-6 yearsReleases progestin to thicken cervical mucus and prevent ovulation
- Often makes periods lighter or stop altogether
- Copper IUD
- Lasts up to 10 yearsNon-hormonal – ideal for those who prefer hormone-free birth control
- May cause heavier periods in the first few months
Birth Control Implant – Over 99% Effective
A small rod placed under the skin of your arm, Nexplanon releases hormones to prevent ovulation and lasts up to 5 years. It is highly effective and convenient.
Sterilization (Tubal Ligation or Vasectomy) – Over 99% Effective
- For Women: Tubal ligation (“getting tubes tied”) permanently blocks the fallopian tubes.
- For Men: Vasectomy cuts the tubes that carry sperm.
Sterilization is permanent, so it is only recommended for people who are sure they do not want children in the future.
3. Best Contraceptive Method: Highly Effective and Convenient Methods
These methods require some effort but still offer strong pregnancy prevention:
Birth Control Shot – 94% Effective
- An injection given every three months.
- Can cause weight gain in some women.
- May delay return to fertility after stopping.
Birth Control Pills – 91% Effective
- Taken daily to prevent ovulation.
- Combination pills (estrogen + progestin) regulate periods and reduce cramps.
- Progestin-only pills (mini-pill) are safer for women who cannot take estrogen.
Birth Control Patch – 91% Effective
- A skin patch changed weekly.
- Works like the pill but with fewer daily reminders.
Vaginal Ring (NuvaRing) – 91% Effective
- A flexible ring inserted into the vagina for 3 weeks at a time.
- Releases hormones similar to the pill and patch.
4. Best Contraceptive Method: Easy and Accessible Methods
If you want a method that is easy to get and does not require a doctor’s procedure, consider:
Male Condoms – 85% Effective
- Protect against both pregnancy and STIs.
- Need to be used correctly every time.
Female Condoms – 79% Effective
- Worn inside the vagina before sex.
- Less effective than male condoms but still provide STI protection.
Withdrawal Method (“Pulling Out”) – 78% Effective
- Requires the male partner to pull out before ejaculation.
- High risk of failure due to pre-ejaculate fluid containing sperm.
5. Best Contraceptive Method: Natural and Hormone-Free Methods
If you prefer birth control without hormones, consider:
Fertility Awareness Method (Natural Family Planning) – 76% Effective
- Involves tracking menstrual cycles and avoiding sex on fertile days.
- Requires careful monitoring and self-discipline.
Copper IUD – Over 99% Effective
- Lasts up to 10 years and does not use hormones.
- Can cause heavier or more painful periods.
Natural methods work best for those who can carefully track ovulation and are comfortable with some risk of pregnancy.
6. Which Method Is Right for You?
To choose the best contraceptive method, ask yourself these questions:
- Do you want a long-term method that you don’t have to think about daily? → IUD, Implant, or Sterilization
- Do you want birth control that also protects against STIs? → Male or Female Condoms
- Are you looking for a non-hormonal option? → Copper IUD, Condoms, or Natural Family Planning
- Do you want a method that helps with period regulation and acne? → Combination Birth Control Pills
- Are you okay with a daily routine? → Birth Control Pills
- Would you prefer something weekly or monthly? → Patch or Vaginal Ring
There is no one-size-fits-all answer. The best birth control is the one that fits your needs and lifestyle.
7. Conclusion
Choosing the right contraceptive method is an important decision. Long-term methods like IUDs and implants are the most effective, while pills and patches offer convenience. Condoms are the best option for STI protection. Always consult a healthcare provider to discuss the best birth control for your specific needs.
References
- Trussell, J. (2011). Contraceptive failure in the United States. Contraception, 83(5): 397–404.
https://doi.org/10.1016/j.contraception.2011.01.021
- Curtis, K. M., et al. (2016). U.S. medical eligibility criteria for contraceptive use. MMWR Recommendations and Reports, 65(3): 1–104.
https://www.cdc.gov/reproductivehealth/contraception/mmwr/mec/summary.html
- Winner, B., et al. (2012). Effectiveness of long-acting reversible contraception. New England Journal of Medicine, 366(21): 1998–2007.
https://doi.org/10.1056/NEJMoa1110855
- Gallo, M. F., et al. (2013). Combination contraceptives and weight gain. Cochrane Database of Systematic Reviews, 2013(1).
https://doi.org/10.1002/14651858.CD008552.pub2
- Hatcher, R. A., et al. (2018). Contraceptive Technology (21st ed.).
https://www.amazon.com/Contraceptive-Technology