The Emotional Toll of Endometriosis Pain
Endometriosis pain isn’t just a physical experience—it can quietly unravel a woman’s confidence, energy, and sense of self. Many, like Julia, spend years feeling like their bodies are betraying them. They miss birthdays, cancel plans, skip work, and sometimes, question their worth.
The emotional weight of chronic pain is heavy. Being dismissed by doctors, misunderstood by friends, or told “it’s just bad cramps” leaves deep emotional scars. Anxiety builds with each new cycle. Depression can creep in when the pain won’t stop. And isolation becomes common when others don’t see what you’re going through.
Julia often smiled through tears. On the outside, she looked “fine.” But inside, she was breaking.
“The hardest part wasn’t just the pain—it was pretending I wasn’t in pain all the time.”
If you’ve ever felt that way, you’re not alone. Your pain is valid. Your story matters. And healing includes your heart and mind—not just your body.
Endometriosis Pain: Finding Hope Through Small Daily Changes
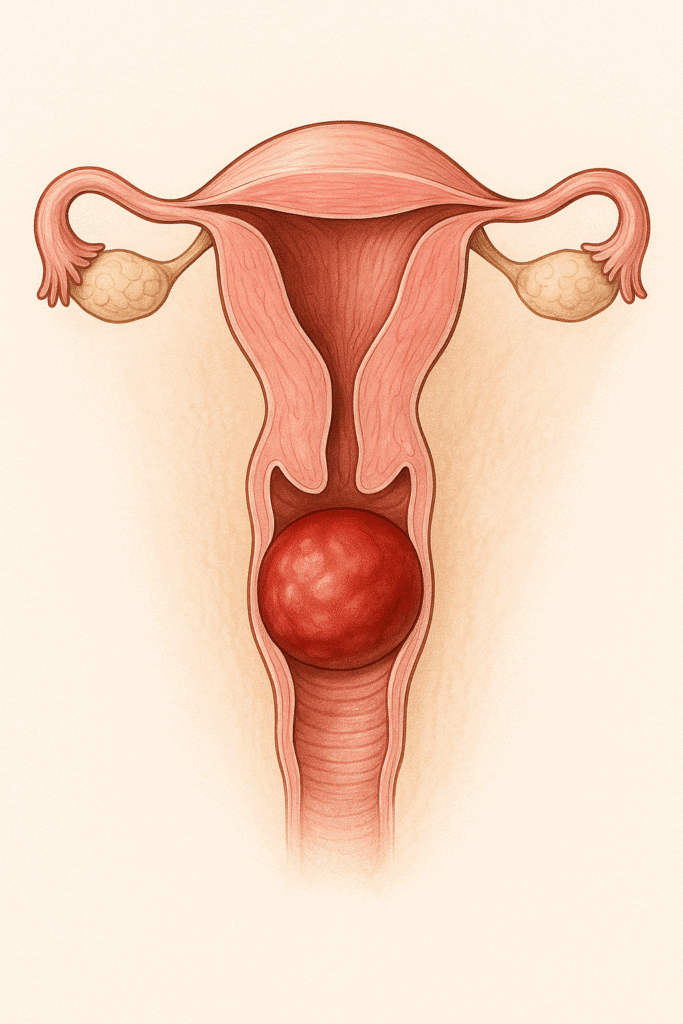
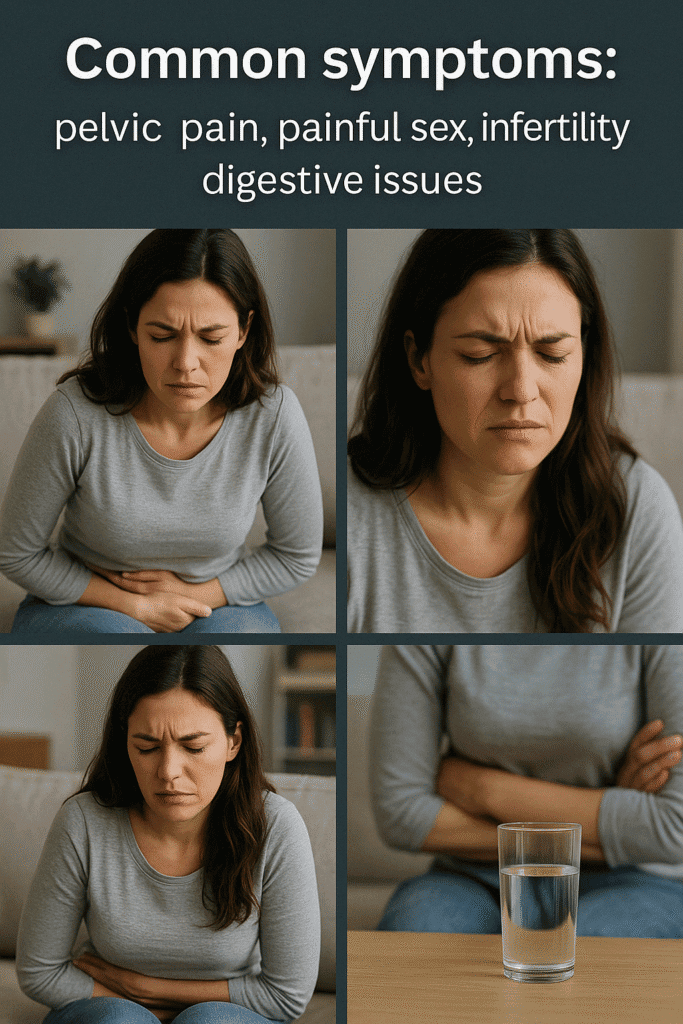
Endometriosis pain is not just physical—it’s emotional, mental, and deeply personal. For millions of women around the world, it’s a silent weight carried through every phase of life. The stabbing cramps, aching lower back, digestive discomfort, and sheer exhaustion aren’t “just bad periods”—they’re a daily reality that can feel overwhelming and isolating.
If you’ve been told to “just deal with it” or offered temporary relief without real answers, you’re not alone. Understanding endometriosis pain goes beyond medical jargon—it’s about connecting the dots between your symptoms, your lifestyle, and your overall health.
One of the most overlooked areas is how food and everyday choices can influence endometriosis pain. While there’s no one-size-fits-all cure, many women have found significant relief by making simple, sustainable changes to their diet and routine.
This guide is for you. Whether you’re newly diagnosed or have been managing this condition for years, we’ll walk through what works, what doesn’t, and how you can take control—one gentle, empowering step at a time.
1. Medical Treatments for Endometriosis Pain Relief: Julia’s Story
When Julia was 28, she found herself curled up in bed every month, missing work, social events, and even her sister’s wedding rehearsal. The pain wasn’t just “bad cramps.” It felt like something deeper—sharp, twisting, and relentless. Doctors dismissed her for years, handing her painkillers and sending her home. But nothing changed.
It wasn’t until a compassionate OB-GYN finally mentioned the word endometriosis that everything started to make sense.
Treating Endometriosis Pain: What Helped Julia (and Could Help You Too)
Medical treatments for endometriosis pain are not about “fixing” you—they’re about reducing the intensity of symptoms and giving you your life back, one day at a time.
Endometriosis Pain-Relieving Medications
For Julia, the first step was learning to treat endometriosis pain early, not after it became unbearable. Over-the-counter anti-inflammatories helped a bit, but some days, she needed prescription-strength medication just to get out of bed. Starting these medications before her period began gave her a little more control.
Hormonal Therapies
After discussing her options, Julia began hormonal therapy—not for birth control, but to manage her endometriosis pain. There are several options, each with pros and cons:
- Hormonal contraceptives helped regulate her cycle, which meant fewer flare-ups and more predictable pain patterns.
- Progestin-based therapies worked to shrink the tissue growing outside the uterus. It took time, but her pain became more manageable.
- Estrogen suppressants gave her even more relief—but came with side effects like mood changes and hot flashes, so her doctor closely monitored her.
It’s important to know that symptoms can return once hormonal treatment stops. Julia had to find the right balance—what worked for her body, her lifestyle, and her mental health.
Note: Symptoms can return after stopping hormonal treatments.
2. Surgical Options for Endometriosis Pain Relief
When Medication Isn’t Enough: Julia Faces a Bigger Decision
Despite months of trying hormonal therapies, Julia still woke up some mornings with sharp, burning pain radiating through her pelvis and lower back. She felt like she was doing everything right—but her body wasn’t responding the way she hoped.
That’s when her doctor gently brought up the next step: laparoscopic surgery.
Laparoscopic Surgery: A Closer Look at Relief
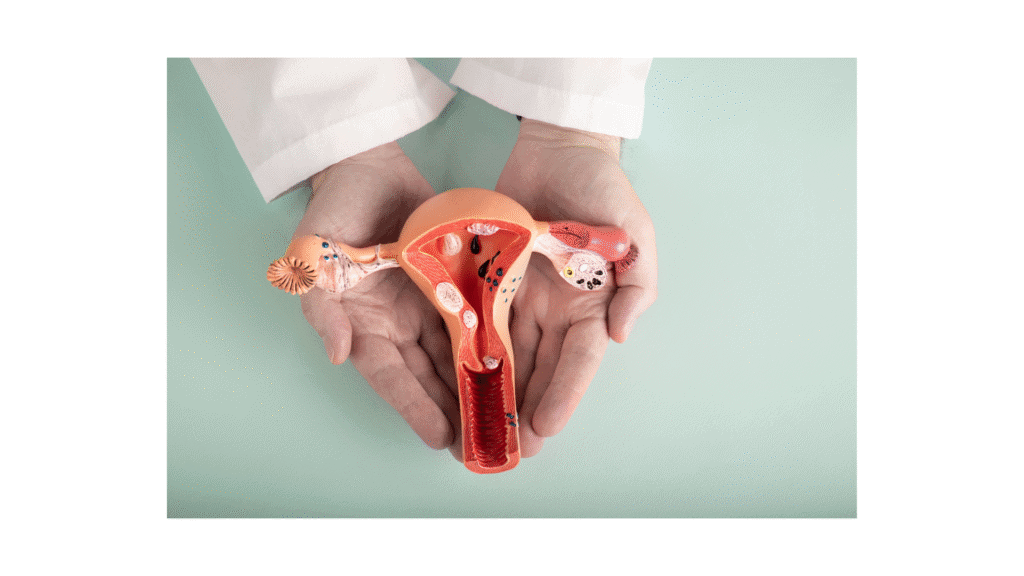
Julia was terrified at first. The idea of surgery sounded extreme. But her doctor explained that laparoscopy is a minimally invasive procedure—tiny incisions, tiny cameras, and expert hands working to remove the endometriosis tissue and scar formations that medications couldn’t reach.
For Julia, the procedure revealed something shocking: endometriosis had wrapped around parts of her bowel and bladder. No wonder she had struggled for so long. The surgeon carefully removed the lesions, and for the first time in years, Julia woke up with a real sense of relief.
Laparoscopic surgery isn’t a cure, but it gave her a fresh start. Her periods became more manageable. Her fatigue eased. She laughed more. She danced again.
“I didn’t realize how much pain I had normalized… until I wasn’t in pain anymore.” —Julia
When Hope Fades: Considering a Hysterectomy
Years later, the pain started creeping back. Not as intense, but enough to disrupt her sleep and affect her daily life. She was older now. She had made peace with not having children. So when her doctor brought up hysterectomy, she didn’t shut down the idea—but she asked questions.
A hysterectomy removes the uterus, and in some cases, the ovaries too. For women with severe, treatment-resistant endometriosis, it can reduce or even eliminate certain types of pain. But it’s not always a cure—especially when endometriosis grows outside the uterus, like in Julia’s case.
After long talks with her doctor and her partner, Julia chose to move forward with the surgery. It wasn’t easy. But she felt empowered—this was her choice, not something forced upon her. Recovery took time, and some symptoms lingered, but she finally felt like she was reclaiming her body.
3. Finding Comfort Beyond Medicine: Julia Discovers Supportive Therapies
After surgery, Julia finally had a window of peace—but like many women with endometriosis pain, she knew that healing wasn’t linear. Some discomfort returned. Not the sharp, unbearable pain from before, but a dull ache that lingered and stole her focus on certain days.
Instead of jumping back into medications, Julia decided to explore supportive therapies—gentler approaches that focused on her body’s healing, not just its symptoms.
Pelvic Floor Physical Therapy: Reclaiming Her Body
Her first stop was pelvic floor physical therapy. At first, Julia felt embarrassed. She had never even heard of it, and the idea of talking about her pelvic muscles made her nervous.
But her therapist was kind, patient, and incredibly knowledgeable. Together, they worked on releasing the tight, overactive muscles that had tensed up from years of guarding against pain. Slowly, Julia started to feel more mobile, less sore, and more in tune with her own body.
“I didn’t know how much my body had been bracing for pain—until it finally relaxed.”
Heat Therapy: Small Acts of Self-Care
Some days, Julia didn’t want to talk or move. On those days, she turned to something simple but powerful: heat therapy. A warm bath. A heating pad tucked under her blanket. It wasn’t fancy—but it helped.
The heat melted away cramping and muscle tension, offering gentle relief that made her feel cared for. It was a reminder that rest was not weakness—it was part of healing.
Acupuncture: A New Perspective
A friend recommended acupuncture, and Julia hesitated. Needles? Really?
But she gave it a try. The sessions were surprisingly peaceful. Soft music. Dim lights. A quiet room where she could just be. Some sessions brought more relief than others, but overall, she noticed her nervous system felt calmer, and her pelvic pain less reactive.
Science is still catching up on how acupuncture works, but for Julia—and many others—it became part of her toolbox for managing endometriosis and pain in a holistic way.
4. Lifestyle Adjustments That Helped Julia Manage Her Endometriosis Pain
After years of battling endometriosis pain with surgeries, hormonal treatments, and medications, Julia realized that healing wasn’t just about what happened in the doctor’s office—it was also about the small choices she made every day.
These lifestyle adjustments didn’t cure her condition, but they helped her reduce the intensity of her endometriosis pain, feel stronger, and reconnect with her body.
Balanced Nutrition: Calming the Inflammation from the Inside Out
One of the first things Julia learned was that endometriosis pain is deeply connected to inflammation. And food, she discovered, could be either a trigger or a powerful ally.
She began making small, consistent changes:
- Adding omega-3-rich foods like salmon, walnuts, and flaxseeds, known to reduce inflammation.
- Eating more leafy greens like kale and spinach to support hormonal balance.
- Switching to whole grains like quinoa and brown rice to stabilize her energy.
- Choosing antioxidant-rich fruits like berries and citrus to fight oxidative stress.
She also limited:
- Processed foods and red meat, which worsened her symptoms.
- Dairy, which seemed to trigger bloating.
- Excess caffeine and alcohol, which made her more sensitive to pain.
Within a few weeks, she noticed a shift—not just in her digestion, but in her endometriosis pain levels. Flares became less intense, and she felt more in control.
Gentle Exercise and Stretching: Moving Without Fear
Julia had long feared that physical activity would make her endometriosis pain worse. But her doctor encouraged her to try low-impact movement, and it changed everything.
Yoga helped her stretch tight muscles without pushing her limits. Swimming made her feel light and free, even on hard days. And walking in the early morning brought peace and clarity.
These gentle exercises boosted endorphins, which acted as natural painkillers. Instead of dreading movement, Julia began to crave it as a part of her healing routine.
Mindfulness and Stress Reduction: Easing the Pain Loop
Living with endometriosis pain often meant living with anxiety. Julia constantly worried about when the next flare-up would strike. Through mindfulness, she learned to quiet that fear.
Simple practices like deep breathing, guided meditation, and CBT (Cognitive Behavioral Therapy) helped her reframe the way she experienced pain. She learned that emotional stress could actually amplify endometriosis pain—and calming her mind could help ease her body.
Journaling, gratitude lists, and even five minutes of stillness each morning became her way of showing up for herself.
Supportive Supplements: Small Boosts That Made a Difference
With her doctor’s guidance, Julia started using natural supplements that supported her healing:
- Vitamin D helped strengthen her immune system.
- Magnesium eased cramping and promoted muscle relaxation.
- Turmeric (curcumin), known for its anti-inflammatory effects, became part of her daily tea ritual.
Though subtle, these supplements became part of her overall plan to manage endometriosis pain from the inside out.
Endometriosis Pain : When Should You See a Doctor?
Julia often blamed herself for not speaking up sooner. She spent years thinking her symptoms were just “normal period pain.” Friends told her to tough it out. Some doctors dismissed her concerns. But endometriosis pain is not normal, and it should never be ignored.
Knowing when to seek medical help can change the course of your journey.
You should absolutely see a doctor if:
- The pain is severe and disrupts your daily life.If you’re missing work, canceling plans, or unable to sleep due to endometriosis pain, it’s time to talk to a specialist. Julia spent too many nights curled up on the bathroom floor, thinking she just needed to push through. But pain that stops you from living isn’t something you should endure—it’s something you deserve relief from.
- The pain persists despite treatment.Have you tried hormonal pills, painkillers, or diet changes with no improvement? That’s a sign something deeper might be going on. Endometriosis can be resistant to certain treatments, and persistent endometriosis pain needs to be re-evaluated.
- You experience painful sex, bowel issues, or infertility.These symptoms aren’t “in your head”—they’re classic signs of endometriosis pain spreading to areas like the pelvic floor, bladder, or intestines. Julia was shocked to learn that her digestive symptoms were connected to her condition all along.
- Your symptoms return after stopping medication.Many women experience a return of endometriosis pain once they stop hormonal therapies. This doesn’t mean the treatment failed—it means your doctor needs to help you find a longer-term plan, possibly including surgery, physical therapy, or lifestyle shifts.
“If I had gone sooner,” Julia reflects, “I might have spared myself years of pain.”
Early diagnosis and treatment can make a world of difference. If something doesn’t feel right—trust your body. Endometriosis pain is real, and your experience matters.
Tracking and Journaling Endometriosis Pain
One of the most empowering tools Julia discovered was tracking her endometriosis pain.
At first, it was just notes on her phone—when the pain started, what she ate, how she slept, her mood. But over time, patterns began to emerge. Certain foods triggered bloating. Stressful weeks led to stronger cramps. Lack of sleep made everything worse.
By keeping a simple journal, Julia gained something she hadn’t felt in years: control.
Journaling helped her communicate more clearly with her doctor. Instead of vague descriptions, she could say:
“The pain starts two days before my period and lasts for five.”
“It worsens after I eat dairy.”
“It’s sharp on the left side after ovulation.”
Her doctor used this data to tailor her treatment and recommend lifestyle adjustments. It also helped Julia prepare emotionally for hard days—and celebrate the good ones.
Apps, notebooks, voice notes—there’s no wrong way to track your symptoms. What matters is listening to your body and honoring what it’s trying to tell you.
“My pain journal didn’t just help my doctor. It helped me trust myself again.”
If you’re living with endometriosis pain, consider journaling as a tool—not just for managing symptoms, but for reconnecting with yourself.
Managing Endometriosis Pain: You Are Not Alone
Endometriosis pain can feel overwhelming, but it doesn’t have to control your life. You don’t have to choose between suffering in silence or living in fear. There is a middle ground—and it starts with knowledge, support, and a plan that works for you.
Throughout her journey, Julia discovered that no single treatment was enough. What helped her was a combination of:
- Medical therapies, like hormonal treatments and eventually surgery
- Supportive care, including pelvic physical therapy and acupuncture
- Daily lifestyle changes, like mindful eating, movement, and supplements
- And above all, emotional healing, through therapy, community, and self-compassion
The most effective way to manage endometriosis pain is with a personalized plan, built around your specific symptoms, needs, and goals. What works for one woman might not work for another—and that’s okay.
“You are not weak. You are not exaggerating. And you are definitely not alone.”
If you or someone you love is struggling with endometriosis pain, don’t wait. Seek a specialist. Build a support system. Keep asking questions. Relief is possible—even if it takes time.
Let Julia’s story be a reminder: healing is not linear, but it is possible. And every step you take—every choice to listen to your body—is a step toward reclaiming your life.
References
-
Coxon, L., et al. Current Developments in Endometriosis-Associated Pain. Cell Reports Medicine, 2024.
-
Tsuei, A., et al. Comprehensive Management of Bowel Endometriosis. Journal of Clinical Medicine, 2025.
-
Saunders, P., et al. Endometriosis: Improvements and Challenges in Diagnosis and Symptom Management. XCRM, 2024.
-
Alonso, A., et al. Medical Management of Endometriosis. Current Opinion in Obstetrics & Gynecology, 2024.
-
Bayu, P., et al. Vitamin C and E Antioxidant Supplementation May Significantly Reduce Pain Symptoms in Endometriosis. PLoS ONE, 2024.