What Is Ovarian Reserve? Siomara’s Fertility Future
By Dr Pereira
What Is Ovarian Reserve? Siomara’s Fertility Future
Siomara was 30 years old, vibrant, full of plans. She had recently gotten engaged and couldn’t stop smiling. Her wedding would be in the spring, and motherhood was part of her dream—just not yet. “Maybe after 35,” she said casually, brushing off the subject as something far off.
But when she sat in my office that day, I gently asked a question that made her pause.
“Siomara, have you ever checked your ovarian reserve?”
She blinked. “What is ovarian reserve?”
That single question became a turning point.
What Is Ovarian Reserve?
A woman is born with 1 to 2 million eggs, but by the time she reaches puberty, only around 300,000 remain. With each menstrual cycle, several eggs are lost, even though only one typically matures for ovulation. As a woman ages—especially after 30 and more rapidly after 35—her egg count declines. But it’s not just about quantity. Egg quality also diminishes over time.
So, what is ovarian reserve? It’s a measure of the quantity and quality of eggs left in a woman’s ovaries. And it’s one of the most important indicators of future fertility. Understanding what is ovarian reserve is key for any woman planning her future.
Why Does It Matter?
For Siomara, like many women waiting to have children later in life, understanding ovarian reserve is essential. It’s not about panic. It’s about information. Knowledge. Control. Knowing what is ovarian reserve provides a realistic roadmap.
Why Ovarian Reserve Is So Important
The concept of ovarian reserve may seem abstract, but its importance is concrete. Here’s why understanding what is ovarian reserve matters:
- It helps predict natural fertility potential: Women with a strong ovarian reserve are more likely to conceive naturally.
- It guides fertility treatment planning: If the reserve is low, time-sensitive treatments like egg freezing or IVF may be recommended.
- It gives insight into menopause timing: While not exact, a diminished ovarian reserve can signal early menopause.
Low Ovarian Reserve Does Not Mean Infertility
This is important: having a low ovarian reserve doesn’t mean a woman can’t get pregnant. Many women conceive with a low reserve, especially when guided by a fertility specialist. But it does mean fewer eggs, and potentially lower quality—so timing and strategy become critical. Understanding ovarian reserve means understanding how time impacts your chances. That’s why it’s essential to ask: what is ovarian reserve and how does it apply to me?
How Do We Test Ovarian Reserve?
Siomara was surprised to learn that testing ovarian reserve wasn’t difficult. In fact, it can be done with a combination of blood work and an ultrasound. Knowing what is ovarian reserve also means knowing how it’s measured.
Hormonal Blood Tests
| Test | What It Measures | Optimal Range |
|---|---|---|
| Anti-Müllerian Hormone (AMH) | Egg supply | 1.0–4.0 ng/mL |
| Follicle Stimulating Hormone (FSH) | Ovarian function | <10 mIU/mL (Day 3) |
| Estradiol (E2) | Ovarian response | 25–75 pg/mL (Day 3) |
| Inhibin B | Follicle activity | >45 pg/mL |
AMH is the most stable marker. It doesn’t fluctuate much during the cycle. FSH and estradiol help give a fuller picture, but they can vary month to month.
Ultrasound Tests
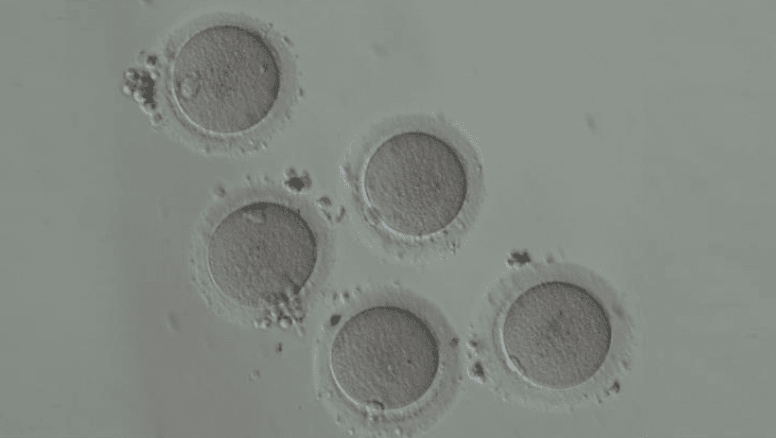
- Antral Follicle Count (AFC): Using a transvaginal ultrasound, we count the small resting follicles in each ovary. A higher count (>12) is considered reassuring. A low count (<5) suggests diminished reserve.
- Ovarian Volume: Larger ovarian size tends to correlate with better reserve.
When I performed Siomara’s ultrasound that same morning, I quietly counted the follicles. Eight on one side, six on the other. Fourteen in total. A healthy number for her age. That’s the value of understanding ovarian reserve—it allows for timely action.
Factors That Influence Ovarian Reserve
The concept of ovarian reserve is dynamic. It’s not the same for everyone, and many variables can affect it. To fully grasp what is ovarian reserve, we must also understand what impacts it.
- Aging
- Natural egg loss accelerates after 30.
- After 35, both quantity and quality drop faster.
- Chromosomal abnormalities in eggs increase with age.
- Lifestyle
- Smoking: Toxic to the ovaries. Advances menopause by up to four years.
- Obesity: Alters hormonal balance and reduces fertility.
- Excessive alcohol: Lowers AMH and damages DNA in eggs.
- Medical Conditions
- Endometriosis: Can damage ovarian tissue.
- PCOS: Often presents with high follicle count but poor egg quality.
- Autoimmune disorders: Can cause premature ovarian failure.
- Family History
If a woman’s mother or sister experienced early menopause, her own reserve may decline sooner than average.
These insights helped Siomara reflect. Her aunt had menopause at 42. That detail suddenly felt more significant. Another reason why knowing what is ovarian reserve can be so impactful.
Can You Improve Ovarian Reserve?
I wish I could promise women like Siomara that a magic pill could increase ovarian reserve. But the truth is:
- We cannot increase the number of eggs.
- We cannot reverse aging.
However, we can protect egg quality, and that makes all the difference. And understanding what is ovarian reserve helps us make these choices wisely.
What Helps
- Coenzyme Q10 (CoQ10): May improve mitochondrial function in eggs.
- Healthy lifestyle: Stop smoking. Eat well. Move your body.
- Stress reduction: Chronic stress can interfere with hormone levels.
- Regular screening: Monitoring AMH and AFC over time.
And most importantly:
- Fertility preservation.
That’s what I recommended to Siomara.
“We can freeze your eggs now while your reserve is healthy. That way, if you decide to wait until after 35, you’ll have better-quality eggs stored.”
She nodded slowly, absorbing the weight of the information. This was not a scare tactic. This was a gift: foresight. This is why understanding ovarian reserve is a cornerstone of reproductive planning.
Real Stories, Real Impact: Why Women Are Asking “What Is Ovarian Reserve?”
Siomara’s case isn’t isolated. Every week, I see women in their late 20s or early 30s who have never heard of the term. Once we explain what is ovarian reserve and how it affects their ability to plan their family in the future, the response is often the same—relief, empowerment, and sometimes a tinge of regret for not knowing sooner.
Understanding what is ovarian reserve is no longer just for women undergoing fertility treatment. It’s a vital part of reproductive awareness—just like learning about ovulation, contraception, or STIs. It’s the kind of knowledge that can shape life decisions. That’s why more gynecologists, endocrinologists, and wellness professionals are starting conversations earlier, especially with women who plan to delay motherhood.
There’s a shift happening—women want control. And to gain control, they need education. They need to ask: what is ovarian reserve, and why does it matter to me, now?
What Is Ovarian Reserve? You Know the Answer
Siomara’s story is not uncommon. Every day, women are postponing motherhood for valid and empowering reasons—careers, relationships, personal growth. But knowing your body is the most empowering step of all.
What is ovarian reserve? It’s your window into reproductive health. It allows you to act in time, to explore egg freezing, to protect your dreams. Understanding what is ovarian reserve is the foundation of that journey.
You don’t need to panic. You just need to plan. And it all starts by understanding ovarian reserve.
Stay tuned for the next post: Egg Freezing Explained: The Science, Success, and Strategy.
Would you like to assess your ovarian reserve? Book a consultation today and learn where you stand.
Share this post and help another woman learn about her fertility future.
References
- American Society for Reproductive Medicine (ASRM). "Ovarian Reserve Testing: What You Need to Know." Fertility and Sterility, 2023. “>American Society for Reproductive Medicine (ASRM). “Ovarian Reserve Testing: What You Need to Know.” Fertility and Sterility, 2023.
- Wallace, W.H.B., & Kelsey, T.W. "Human Ovarian Reserve from Conception to Menopause." PLoS ONE, 2010. “>Wallace, W.H.B., & Kelsey, T.W. “Human Ovarian Reserve from Conception to Menopause.” PLoS ONE, 2010.
