Hidden Endometriosis: Imagine living your life without pain, with regular cycles, and no signs of trouble — until one day, you notice a small lump. That was the reality for a 37-year-old woman who walked into a gynecology clinic thinking she had a simple cyst. But what doctors discovered was something much rarer: endometriosis presenting as a vaginal mass.
Most people think of endometriosis as a condition that causes pelvic pain, heavy periods, or infertility. But sometimes, it hides in the most unexpected places, causing unusual symptoms that can delay diagnosis.
Endometriosis is often described as a condition that hides in plain sight. While many women experience painful periods and pelvic discomfort, some carry a more elusive version of the disease — one that defies expectations and challenges diagnosis. This is the reality of hidden endometriosis.
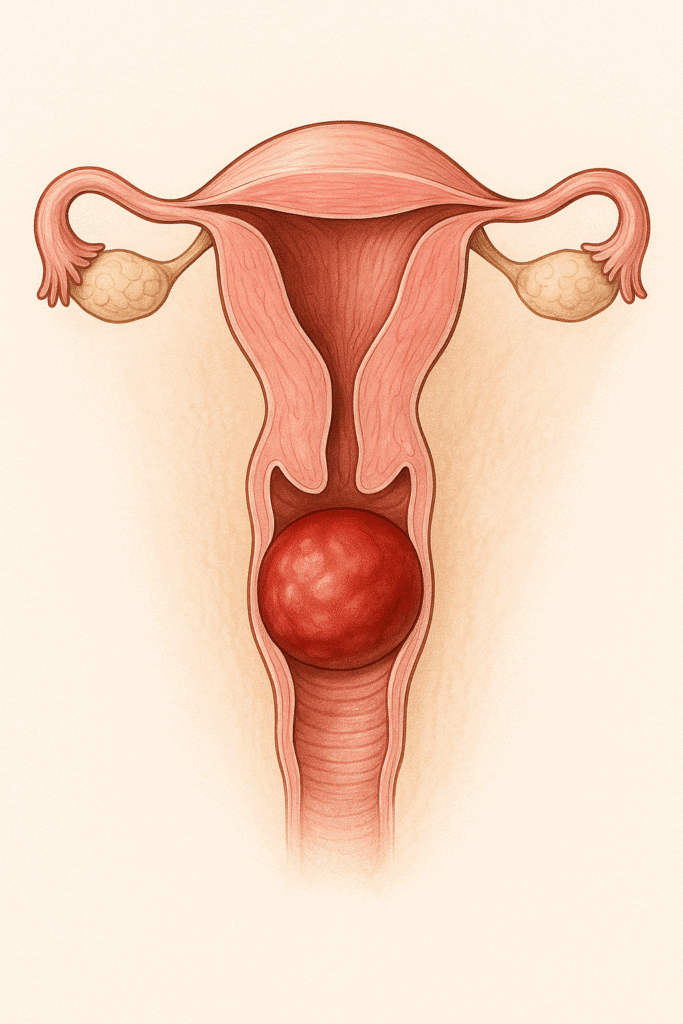
In most cases, endometriosis is found on the ovaries, fallopian tubes, or pelvic peritoneum. But in rare and surprising scenarios, it can implant in locations far beyond — even in the vaginal wall, abdominal muscles, or distant organs. When this happens, symptoms often don’t match what doctors typically look for, and imaging may offer little help. Women are left with unanswered questions, misdiagnoses, and years of unnecessary suffering.
In this real and striking case, a woman experienced pain during sex and an unusual sensation of pelvic pressure. No one suspected what was really going on — not until surgery revealed endometrial tissue growing inside her vaginal wall. This discovery not only brought her long-awaited answers, but also highlighted a crucial medical truth: hidden endometriosis can be silent, but not harmless.
During the operation, they found a cyst containing “chocolate-colored” fluid — a telltale sign of endometriosis. Pathology confirmed: it was an endometriotic cyst in the vaginal wall.
The woman recovered well after surgery and remained symptom-free three months later.
Her journey matters. And by sharing it, we hope to raise awareness, shorten diagnostic delays, and give voice to the women whose pain deserves to be taken seriously.
Hidden Endometriosis: Why is this case important?
Because endometriosis is often thought of as a pelvic disease, many don’t realize it can appear outside the uterus, even in the vagina — a location reported in only 0.02% of endometriosis cases.
Doctors usually suspect other conditions when facing a vaginal mass: Gartner’s cyst, urethral diverticulum, Skene’s gland cyst, Bartholin’s cyst, or even a tumor. Endometriosis is rarely on the list.
That’s why diagnosis often depends on surgical removal and histology (examining tissue under a microscope).
What does this mean for women?
If you’ve been diagnosed with endometriosis, or have unexplained pelvic symptoms, remember:
endometriosis can be sneaky. It can hide in scars, on the bowel, bladder, even in the lungs — and in rare cases, in the vaginal wall.
Early recognition and treatment can improve quality of life. In this woman’s case, a small mass caused growing discomfort and affected intimacy. Surgery resolved her symptoms.
Takeaway message
If you notice a lump, discomfort, or unusual symptoms in your intimate area — seek medical advice. Not every lump is dangerous, but every lump deserves attention.
Endometriosis may be more common than we think — and sometimes, it hides in the most unexpected places.
References
- Nelson P. Endometriosis presenting as a vaginal mass. BMJ Case Rep. 2018;2017:bcr-2017-222431.
https://doi.org/10.1136/bcr-2017-222431
- Giudice LC. Endometriosis. N Engl J Med. 2010;362(25):2389-2398.
https://doi.org/10.1056/NEJMcp1000274
- Vercellini P, Vigano P, Somigliana E, Fedele L. Endometriosis: pathogenesis and treatment. Nat Rev Endocrinol. 2014;10(5):261-275.
https://doi.org/10.1038/nrendo.2013.255
- Kennedy S, Bergqvist A, Chapron C, et al. ESHRE guideline for the diagnosis and treatment of endometriosis. Hum Reprod. 2005;20(10):2698-2704.
https://doi.org/10.1093/humrep/dei135
- Redwine DB. Was Sampson wrong? Fertil Steril. 2002;78(4):686-693.
https://doi.org/10.1016/S0015-0282(02)03356-5
This content is for educational purposes only and does not replace professional medical advice. Always consult your healthcare provider.
