Understanding IVF: The Beginning of Edgard and Patricia’s Journey
By Dr Pereira
“Doctor, we’ve tried everything,” Patricia began, her voice trembling. “Ovulation kits, vitamins, tracking apps… but still no baby.”
Edgard sat beside her, silent but supportive. He squeezed her hand as I reviewed their medical file. They had been trying to conceive for two years. Patricia’s tests came back normal, but Edgard’s semen analysis revealed low sperm count and reduced motility.
That day marked the beginning of their journey into understanding IVF.
What Does Understanding IVF Really Mean?
IVF stands for In Vitro Fertilization, a process where eggs and sperm are combined outside the body to create embryos. For couples like Edgard and Patricia, understanding IVF means more than memorizing steps; it’s about emotionally preparing for a journey that involves patience, science, and hope.
Understanding IVF is important for:
- Women with blocked or damaged fallopian tubes
- Women with poor egg quality or low ovarian reserve
- Couples with unexplained infertility
- Men with low sperm count or poor sperm motility
- Those with genetic conditions requiring embryo testing
- LGBTQ+ couples and individuals using donor eggs, sperm, or surrogates
Edgard and Patricia checked more than one of these boxes. They were ready to begin.
Step 1: Ovarian Stimulation
“To increase your chances of success,” I explained to Patricia, “we need more than one egg.”
She would begin daily hormonal injections for 10 to 14 days. These medications stimulate the ovaries to produce multiple follicles instead of just one.
We monitored her closely with:
- Ultrasounds, to measure follicle size and number
- Blood tests, to track hormone levels
When her follicles reached 17–20 mm, we administered a final trigger injection of hCG. This step is crucial in understanding IVF, as timing affects egg quality and quantity.
Step 2: Egg Retrieval
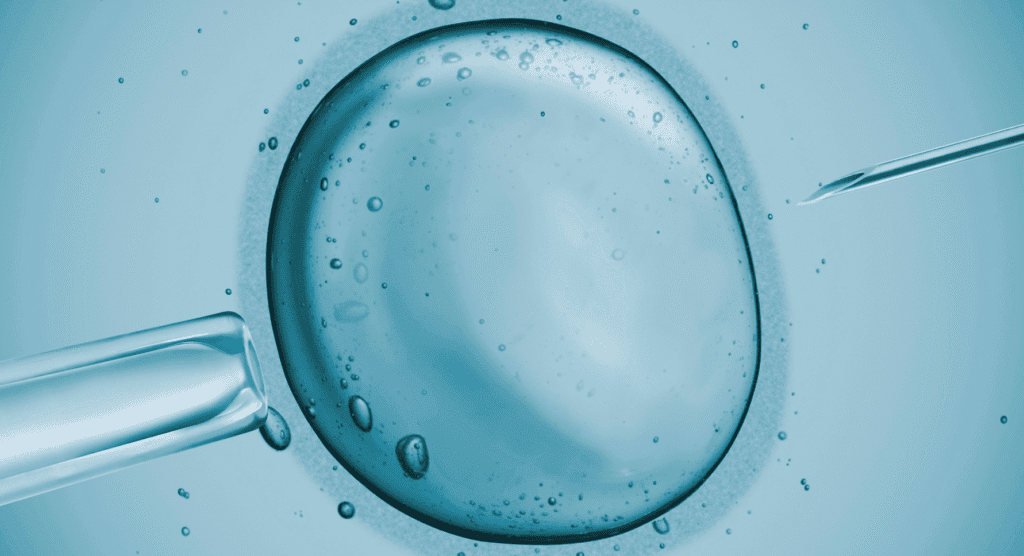
Exactly 36 hours after the trigger shot, Patricia returned for the egg retrieval procedure. Guided by ultrasound, we used a thin needle to gently aspirate the eggs through the vaginal wall.
It was a quick, 15- to 20-minute outpatient procedure under light sedation. She felt no pain, only relief that one major step was over.
That morning, Edgard provided a sperm sample. Because of his low count, we chose ICSI (Intracytoplasmic Sperm Injection), where a single healthy sperm is injected directly into each egg. This part of understanding IVF can feel intimidating, but it’s often the best approach in male factor infertility.
Step 3: Fertilization and Embryo Development
Over the next five to six days, the fertilized eggs developed into embryos. Our embryologists monitored them for quality, cell division, and development.
On Day 5, we had three healthy blastocysts ready. The rest were frozen for future use. Understanding IVF involves preparing for today and tomorrow—because not every cycle results in a pregnancy, and backups matter.
Patricia and Edgard chose to transfer one embryo to reduce the risk of twins. The procedure was simple: a soft catheter placed the embryo into her uterus in less than 10 minutes.
She rested for a few minutes and went home. And so began the hardest part of understanding IVF: the wait.
The Two-Week Wait: Patience and Hope
Those 12 days felt like 12 months. Patricia tried to stay calm. She avoided Google, walked gently around the block, and whispered hopeful thoughts to her belly.
Understanding IVF also means understanding how emotional this phase is. Every twinge, every symptom, becomes a guessing game. We tell patients not to test early. But many do. That’s human. That’s hope.
On Day 12, Patricia took her blood test. Her hCG was positive.
She was pregnant.
Understanding IVF: Emotional Highs and Unexpected Risks
The day after Patricia’s positive pregnancy test, she sat quietly in my office.
“I thought I would feel nothing but joy,” she said. “But I’m still scared.”
IVF Success Rates: What to Expect
Understanding IVF also means managing expectations. Success rates depend on several factors:
- Age of the woman: Younger women have better success.
- Egg and sperm quality: Poor quality lowers chances.
- Embryo quality: Chromosomal abnormalities affect implantation.
- Uterine health: Fibroids, thin lining, or inflammation may interfere.
- Lifestyle: Smoking, obesity, stress all reduce success.
Here’s a rough guide by age:
- Under 35: 45–70%
- 35–37: 40%
- 38–39: 30–35%
- 40–42: 8–25%
- Over 42: Less than 10%
Because Patricia was 34 and we transferred a top-grade embryo, her chances were strong.
That’s when I reminded her: understanding IVF isn’t only about the technical steps—it’s also about embracing the emotional rollercoaster and acknowledging the real risks that come with it.
Let’s walk through them together.
1. Ovarian Hyperstimulation Syndrome (OHSS)
One of the most serious risks in the IVF journey is OHSS, a condition that can occur when the ovaries over-respond to stimulation medications. While most women have mild symptoms, a few experience something more intense.
Mild OHSS may include:
- Abdominal bloating
- Mild weight gain
- Nausea and fatigue
But in rare cases, severe OHSS can cause:
- Rapid abdominal distension
- Difficulty breathing due to fluid buildup
- Blood clots or kidney issues
Understanding IVF means knowing how your body might react. That’s why we tailor stimulation protocols carefully, especially for women with polycystic ovary syndrome (PCOS) or those who respond quickly to hormones.
When Patricia began bloating and felt uncomfortable walking, we acted fast—adjusting her medications and adding fluids. She was lucky. No hospitalization was needed. But she understood the seriousness.
2. Multiple Embryo Transfer and Twin Pregnancies
Many couples come to me asking for two embryos to be transferred. “Twins would be a blessing,” they say.
But here’s the truth: understanding IVF includes knowing that twin pregnancies carry higher risks—for both mother and babies. These include:
- Preterm birth
- Low birth weight
- Gestational diabetes
- Cesarean section risks
With advances in embryo freezing and blastocyst selection, single embryo transfer (SET) is now preferred in most cases.
For Patricia and Edgard, we transferred one excellent embryo. And when that pregnancy test turned positive, they were grateful we prioritized safety.
3. Emotional and Mental Toll
Perhaps the most underestimated part of understanding IVF is the emotional burden.
The injections. The ultrasounds. The waiting. The uncertainty. And yes, the hope—which rises and falls with every test, every phone call, every day.
Patricia once said, “It feels like I’m living in two realities—half hope, half fear.”
She isn’t alone.
Many patients experience:
- Mood swings
- Sleep disturbances
- Anxiety or depression
- Relationship strain
Counseling can help. Support groups are invaluable. And acknowledging that this is not an easy path makes all the difference.
4. Physical Side Effects of IVF Medications
During the ovarian stimulation phase, the body goes through hormonal shifts that can cause side effects like:
- Breast tenderness
- Hot flashes
- Headaches
- Mood changes
While temporary, these symptoms are real and can impact a woman’s daily functioning.
Understanding IVF also means learning how to cope—through hydration, rest, and clear communication with your care team.
5. IVF Failure and Grief
Perhaps the hardest part to talk about: what happens when IVF doesn’t work?
Even with perfect embryos and perfect timing, some cycles fail. When the two-week wait ends with a negative test, it feels like a small death—of a dream, a possibility.
Couples may feel:
- Guilt (“Did I do something wrong?”)
- Anger (“Why us?”)
- Despair (“How much more can we take?”)
This is why understanding IVF means more than memorizing statistics. It’s preparing emotionally—for both the joy and the heartbreak.
Some couples need to take a break. Others move straight into the next cycle. There’s no wrong answer—only what feels right for you.
Understanding IVF: Cost, Accessibility, and Making It Possible
When Edgard and Patricia began their IVF journey, one of their first concerns was cost.
“Doctor,” Edgard asked quietly, “can we actually afford this?”
Understanding IVF means recognizing that finances play a major role—not just in deciding to start, but in sustaining hope through the process.
Let’s break down the reality.
Global Costs of IVF
The cost of a single IVF cycle can vary significantly depending on the country, clinic, and services included. Some centers bundle medication, monitoring, and procedures into one fee—others bill separately.
Here’s a general breakdown by region:
| Country | Average Cost per Cycle (USD) |
|---|---|
| United States | $12,000 – $25,000 |
| United Kingdom | $7,000 – $10,000 |
| Canada | $10,000 – $15,000 |
| Australia | $7,000 – $9,000 |
| Brazil | $4,000 – $6,000 |
| India | $2,000 – $4,000 |
In some places, government subsidies or insurance plans partially cover treatment—but most couples still pay a significant amount out of pocket.
Understanding IVF includes preparing for not one, but potentially multiple cycles. Success may not come on the first try, and costs can multiply fast.
What’s Included in IVF Costs?
When Edgard and Patricia received their first invoice, they were surprised by how many components were listed:
- Consultations and baseline tests
- Hormonal injections and medications
- Ultrasound monitoring and bloodwork
- Egg retrieval and anesthesia
- ICSI (if needed)
- Embryo culture and blastocyst monitoring
- Embryo transfer
- Embryo freezing and storage (optional)
- Pregnancy test and early monitoring
In some cases, additional services like PGT-A (genetic testing) or assisted hatching may be recommended, raising the final cost.
Understanding IVF also means knowing what’s optional and what’s essential, based on your medical history.
Insurance Coverage and Public Access
In a few countries—like Canada, the UK, and parts of Europe—IVF may be partially or fully covered by public health systems, especially for patients who meet specific criteria (age limits, no prior children, or specific diagnoses).
In the U.S., only a few states mandate insurance coverage for infertility, and plans vary greatly. In developing nations, low-cost IVF programs are emerging, but access remains limited for many.
Understanding IVF includes checking local regulations, employer benefits, and fertility financing programs early on.
Cost-Saving Strategies
Many couples explore creative ways to ease the financial burden of IVF:
- Medication discounts or bulk-order pharmacies
- Fertility grants and nonprofit aid programs
- Payment plans offered by clinics
- Traveling abroad for lower-cost IVF (“fertility tourism”)
However, cheaper isn’t always better. Understanding IVF also means ensuring your clinic is reputable, your embryologists are experienced, and your protocol is individualized.
Emotional and Financial Overlap
For Patricia, the cost wasn’t just about dollars.
“It’s not just money,” she told me. “It’s everything we’ve put into this—time, pain, energy, and hope.”
Financial pressure adds to the emotional toll of IVF. That’s why many couples benefit from counseling, not just during treatment, but also while planning how to pay for it.
Understanding IVF is about the whole picture—emotional, physical, and financial.
Understanding IVF: Is It the Right Path for You?
As we closed our final consultation, Patricia looked up with wide, tearful eyes.
“Doctor,” she asked softly, “if this doesn’t work, does that mean we’ll never be parents?”
That question breaks my heart every time. Because understanding IVF isn’t just about needles, scans, or lab results. It’s about real people making the hardest decision of their lives—with love, hope, and often heartbreak.
Who Should Consider IVF?
IVF isn’t always the first step—but it can be the best option for many couples or individuals who’ve tried other treatments without success.
You may want to consider IVF if:
- You’ve been trying to conceive for over a year with no success (or 6 months if over 35)
- You have a known issue like blocked tubes, endometriosis, or male factor infertility
- You’ve experienced multiple miscarriages
- You need to use donor sperm, donor eggs, or a gestational carrier
- You have a medical condition requiring genetic testing (PGT-A or PGT-M)
- You’re freezing embryos for future use (e.g. cancer treatment or delayed motherhood)
Understanding IVF means seeing it not as a last resort, but as a powerful tool. One backed by science, experience, and individualized care.
Weighing the Emotional Cost
One of the most important parts of understanding IVF is preparing emotionally. It’s not a linear path—and it’s not always easy.
- You may face disappointment after a failed cycle.
- You may question your body, your choices, or even your relationship.
- You might grieve an embryo that didn’t implant, or a pregnancy that didn’t continue.
That’s why I always recommend psychological support. Whether it’s a counselor, a support group, or honest conversations with your partner, mental wellness is crucial throughout the IVF process.
Patricia once told me: “I felt like I was losing myself in hormones and numbers. Until I remembered why we were doing this—for love.”
Making a Financial Plan
We talked about IVF costs earlier. But the decision isn’t just about saving money. It’s about creating a strategy:
- Will you try just one cycle, or are you open to two or three?
- Will you freeze extra embryos for future use?
- Do you want genetic testing to reduce miscarriage risk?
- Will your insurance cover part of the cost?
Understanding IVF includes thinking long-term. Sometimes patients need to take a break between cycles—emotionally, physically, or financially. That’s okay.
Alternative Paths
IVF doesn’t work for everyone. And for some couples, it’s not the right fit.
If multiple cycles fail, we may discuss:
- Egg or sperm donation
- Embryo adoption
- Surrogacy
- Traditional adoption
Understanding IVF means understanding its limits—and embracing the many paths to parenthood that still lie ahead.
What Edgard and Patricia Taught Me
They were brave. They asked questions. They cried. They held each other. And when Patricia saw those two pink lines, she didn’t scream—she whispered.
“We made it.”
That’s what understanding IVF is really about. It’s about holding onto hope when science feels overwhelming. It’s about turning information into action, and action into life.
If you’re considering IVF, know this: You’re not alone. Millions of families began where you are now—scared, curious, and searching for answers.
Talk to a fertility specialist. Get the facts. Ask the hard questions. And when you’re ready, take the first step.
You deserve answers. You deserve support. You deserve a chance.
References
- Practice Committee of the American Society for Reproductive Medicine (ASRM). "Assisted Reproductive Technology Success Rates." Fertility and Sterility, 2023.“>Practice Committee of the ASRM. “Assisted Reproductive Technology Success Rates.” Fertility and Sterility, 2023.
